Syphilis is a preventable and curable bacterial sexually transmitted infection (STI). If untreated, it can cause serious health issues. Many people with syphilis do not have symptoms or do not notice them. Syphilis is transmitted during oral, vaginal and anal sex, in pregnancy and through blood transfusion. In 2008, the WHO said that 10.6 million cases of this sexually transmitted genital ulcerative illness that can be cured were reported around the world. The problem is still a big health issue in both the US and Europe. In the UK, the number of cases dropped sharply in the 1980s. From 1998 to 2008, however, the number of cases rose quickly. A disproportionate amount of cases are found in MSM in the UK, and most of the infections are in people over 25. However, there have been recent outbreaks in young heterosexuals. Men are much more likely than women to be diagnosed, but this is mostly because of the high rate in MSM. Early cases of contagious syphilis are tracked in the UK, the USA, and other places.
When you get syphilis, you get infected with the spirochete bacteria Treponema pallidum subsp. pallidum. Other types cause Yaws and Pinta. It can only live for a short time without its host (obligate human parasite).
Syphilis can be passed from person to person through sexual contact with an infected wound, sharing needles or blood products that are infected, or from mother to child through the uterus at any point during pregnancy. Sexual touch can happen through the anogenital area or through the mouth.
Clinical features
Primary syphilis
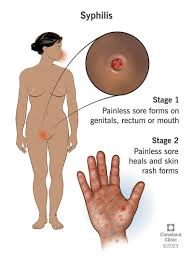
- Characterized by a clear serum-exuding chancre (ulcer), usually solitary, indurated, and painless with a clean, moist foundation. Usually, the anogenital area contains the chancre.
- When ulcers are numerous, painful, purulent, or destructive, and they can mimic an HSV infection, this can lead to an atypical presentation.
- They may also be extragenital, mainly oral, and infrequently occur in the fingers, hands, arms, and other regions. Seldom is Follman’s balanitis reported
- Regional lymphadenopathy is linked to the original lesion.
- Occurs 3–8 weeks (on average) after infection and disappears after 9–90 days. possibly ignored by the patient, especially if it is painless
Secondary syphilis
Illness spread haematogenously results in multisystem involvement during the first two years of illness. Features include:
- Rash: Papular, maculo-papular, generalised macular disease that frequently affects the palms and soles. Though often the rash is not irritating, persons with dark skin may experience itching.
- Condylomata lata: papular wart-like lesions found in damp places, particularly around the anus and vulva.
- Eighty percent of individuals will have skin lesions (rash, condylomata lata)
- An inguinal or generalised lymphadenopathy (in 60% of individuals).
- 30% of patients had mucous membrane lesions in the anogenital, laryngeal, or oral cavities. White bordered ulcers can combine with other lesions to generate “snail track” ulcers.
- Less frequently (less than 10% of patients): hepatitis, glomerulonephritis, periostitis, meningitis, splenomegaly, patchy alopecia, and cranial nerve palsies
Latent syphilis
Defined as T. Pallidum positive serology without any symptoms. Should it occur within the first two years of infection, it is categorized as early latent illness. It is then described as late latent syphilis.
Symptomatic late syphilis
Happens more than two years after the first infection. One-third or so of patients with untreated syphilis will reach this clinical stage.
Gummatous: onset can occur more than 40 years after original infection, however it usually starts 15 years after infection. Gumma are destructive nodular, granulomatous lesions brought on by remaining treponemes reactivating.
Not that they are infectious. The visceral, mucosal, and musculoskeletal systems are all impacted by lesions.Usually developing ten to thirty years following infection, cardiovascular syphilis
Further classifications of neurosyphilis include meningovascular neurosyphilis (which manifests 2–7 years after infection), general paresis (which manifests 10–20 years after infection), and asymptomatic (which can manifest early or late in the disease). The range of neurological disorders is greatly overlapped.
Congenital syphilis
Early years: The first two years of existence
- Absence of growth
- Mucosal lesions include nasal cartilage loss and perforation, which can develop from snuffles and hemorrhagic rhinitis.
- Skin: syphilitic pemphigus blistering bullous lesions, rash (particularly around the mouth and body orifices) about the anus and genitalia, condylomata lata
- Broad lymphadenopathy and hepatosplenomegaly
- Osteochondritis, periostitis pseudoparalysis of the bone
- Other; glomerulonephritis; neurological and ocular complications; haemolysis and thrombocytopenia
Late Age
more than two years of age. Sixty percent will be diagnosed on serology and have no clinical symptoms.
Informations:
- Frontal bossing, short maxilla, high palatal arch, mandibular protuberance, saddlenose deformity, and circumoral rhagades (skin fissures or linear scars)
- Hutchinson’s incisors and Mulberry (Moon’s) molars
- Skeletal: nodules usually of long bones, as the Sabre tibia, or bony sclerosis
- An inflammation is interstitial keratitis.
- Deafness
- Clutton’s joints: typically knee-joint painless effusion on both sides.
- In addition, paroxysmal cold hemaglobinuria, involvement of the gums or neurological system
Diagnosis
The features listed above should be sought for during a comprehensive clinical history and examination. Search the past for clues of a potential infection, such as a history of miscarriages or stillbirths. If an early infection is suspected, special care should be taken in looking for indications of primary and secondary syphilis in the genitalia, skin, and lymph nodes. Examination of every system is required if late or congenital syphilis is suspected.
Co-infection of HIV and syphilis
When infectious syphilis is present, the chance of contracting HIV rises, and syphilis makes HIV more easily spread. Considering that the illnesses frequently coexist, HIV testing is advised.
While the clinical signs of early syphilis in HIV-positive and HIV-negative patients may be same, HIV-infected patients may have larger, deeper, or numerous genital ulcers.
Early syphilis patients infected with HIV may be more likely to have neurological problems.
Each stage of infection should receive the same treatment as those without HIV. Although there is little research to support it, some doctors will provide HIV-positive patients the choice of a neurosyphilis treatment course at any stage of the infection. HIV co-infected patients should be followed up with six monthly serology (3 monthly in an epidemic setting).
External link for further study

