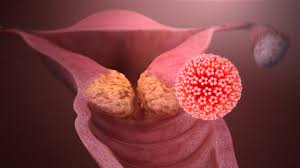
The human papillomavirus (HPV) that is spread through vaginal contact is the most common sexually transmitted virus in the world. Anogenital warts, also known as condylomata acuminata or genital warts, cause a lot of pain and illness and cost a lot of money to treat.
Aetiology and epidemiology
- Anogenital warts are caused by the human papillomavirus (HPV), which infects the skin in many places on the genital area.
- There are more than 100 forms of this double-stranded DNA virus. However, about 90% of anogenital warts are caused by types 6 and 11, which are considered “low risk” because they don’t cause cancer.
- There are at least 13 types of HPV that are “high risk” or can cause cancer. About 90% of anal cancers, at least 12% of oropharyngeal cancers, and 40% of cancers of the external genitalia (penis, vulva, and vagina) are caused by oncogenic HPV types.
- Most sores are harmless, but some anogenital warts will be infected with types of HPV that can cause cancer.
- Infection starts in the basal cells of the epithelial and moves to abnormal cell growth on the skin’s surface, which can be seen as a wart.
- For guys, the peak age is 25 to 34, and for women, it’s 20 to 24.
- The average incubation period is three months, but it can be much shorter or much longer. This long dormant period is important to keep in mind when talking to people who are worried about cheating on their partner.
- One study found that up to half of sexually active people have genital HPV.
HPV is more likely to be found in people who smoke, have hormonal problems (like pregnancy), or have weak immune systems.
Transmission - Anogenital warts are mostly spread through sexual contact with sores or fluids from the genital area that carry viruses. Micro-tears in the recipient’s skin let the virus get to the basal epithelial cells.
- Non-penetrative sex and oro-genital touch are both ways that the virus can be spread.
Digital to genital transfer can also happen from time to time. HPV can be passed from mother to child. When kids get digital warts, they can spread to their genital area. If a child has anogenital warts, you should think about sexual abuse. - Perianal warts can happen even if you have never had anal sex. They are common in both men and women, but they happen more often in MSM. People who have penetrative anal sex may get warts in the anal canal.
- HPV is very contagious, and getting it goes up with the number of sexual partners you have. 60% of messages sent between partners are sent.
- Most HPV infections are not severe; more than 90% of people who are sick will not have any visible lesions (warts).
- 30% of people experience spontaneous decline in 6 months, and by 2 years after infection, HPV DNA can no longer be found in over 90% of people.
Symptoms and signs
Symptoms - Most people come in with sexual lumps or growths.
Most warts don’t hurt, but they can itch or irritate the skin and bleed (anal, cervical, or urethral sores). - The urinary stream can become obstructed by urethral warts. Anogenital warts usually don’t cause many physical complaints, but people who have them often find them very upsetting mentally.
Signs - There can be one or more warts, raised or flat (papular), hard or soft.
- They can have a broad base or pedunculated bases, and their skin can be plain or colored.
- Warts that are keratinized tend to show up on dry skin that bears hair (like the labia majora and scrotum), while warts that are soft and not keratinized tend to show up on warm, wet areas (like the vaginal introitus).
- Most warts are less than 10 mm across, but they can join together to form bigger sores.
On the cervix, vagina, urethral meatus, and anal canal, there may be tumors that don’t cause any symptoms. - Lesions can also be seen in places other than the genital area, like the mouth, throat, eyes, and nose.
Diagnosis
- The diagnosis is based on how the person looks (a naked eye exam).
- Atypical or worrisome growths should be biopsied with a local anesthetic.
- Exam: To look at the anogenital area, use a good light. Do a vaginal speculum on women.
- Proctoscopy is not usually done on people with external anogenital warts unless they are having anorectal complaints.
- Write down the location(s), spread, number, and shape of the warts. It can be helpful to write this down on a genital map.
Special situations - When you’re pregnant, warts may show up or get bigger. There is a 1 in 400 chance that the baby will develop juvenile laryngeal papillomatosis if there are warts present at birth.
- This risk doesn’t seem to go down with treatment, and genital warts often go away on their own during pregnancy. You can give cryotherapy. You shouldn’t use imiquimod (not allowed) or podophyllotoxin (may cause birth defects).
- People with weak immune systems, like those with HIV or diabetes, don’t respond as well to treatment and are more likely to return.
Management
General - The goal of treatment is not to get rid of HPV, but to get rid of warts that can be seen.
Since settlement on its own is likely to happen, there is no way to treat it anywhere. - Treatment is chosen based on the shape, location, and number of lesions, as well as the patient’s preferences and the rules in place in the area.
- Treatment can last anywhere from one to six months, and there are high rates of failure and return with all of them.
- Treatment may not work as well on smokers as it does on non-smokers.
- 10–20% of people who are identified with anogenital warts will also have other STIs, so testing for STIs should be available.
Treatment - Intravaginal and intra-anal warts don’t need to be treated unless they cause pain.
Trichloracetic acid (TCA), electrosurgery, and laser treatment are treatments that aren’t used as often.
Women who have anogenital warts shouldn’t change how often they get their cervix checked. If there is a clinical worry about cervical lesions, you should get a colposcopy.
Follow-up and PN - It is not a good idea to look up former sexual partners.
- Treatment of sexual partners has no effect on how the infection in the index patient develops over time. However, present partners can be offered STI screening and information about the condition.
- There is a lot of different information but using a condom may help protect against getting HPV and may even help when both partners are infected by preventing them from being exposed to the virus again.
- People who are in a lot of mental pain may need to be referred to a counselor.
Vaccination
To help protect against cervical cancer, the UK, Australia, and the USA all have programs where people can get vaccinated against HPV. Gardasil® is a four-valent HPV vaccine that has been used in Australia since 2007 and came out in the UK in 2012. It protects against HPV types 6, 11, 16, and 18. This seems to have made a big difference in lowering the number of people who have genital warts.
Cervical Screening - Cervical screening is a way to find cervix diseases that aren’t yet cancerous. It has been proven to be an effective way to lower the number of cases and deaths from cervical cancer. Death rates from squamous cell cervical cancer in the UK have dropped by 7% a year since the call/recall program for cervical screening began in the 1980s.
- UK call and recall schedule: Up until recently, screening practices varied across the UK. However, the UK National Screening Committee has suggested that all screening should start at age 25, which is what happens in England and Northern Ireland.
| First invitation (age) | 25 years |
| Routine recall | 3 yearly between 25 and 49 and then 5 yearly until 65 years |
- In the UK, all cervical screening is done using liquid-based cytology technology. This is better than traditional cytology in a number of ways, such as having a higher sensitivity and fewer tests being recorded as inadequate.
- The cytological test called dysskaryosis can show either low grade or high grade dyskaryosis, which means it is moderately or severely invasive squamous cancer.
CIN is a histological finding that is broken down into stages 1–3 that are linked to worsening dyskaryosis.
The method: A speculum test is used to see what the cervix looks like. The sample should come from the transition zone, which is where the squamocolumnar junction is. A brush is put inside the cervix to take the sample. The center bristles are put into the endocervical canal, and the brush is turned five times counterclockwise. This is important if you want to get a lot of cells. For some sampling kits, the brush head needs to be broken off and put into a vial of fixative (like SurepathTM). For others, the brush needs to be rinsed in the vial and pushed against the bottom of the vial at least 10 times to spread the bristles apart (Thinprep®).
HPV screening
Research has shown that women who have no cytological problems and are HPV negative six months after treatment for CIN can safely go back to their regular screenings every three years. In England, pilot tests are being done to see if HPV testing should be added to the cervical screening program. In 2012, all women in Scotland who had been treated for CIN 1, 2, or 3 had to get an HPV test as a “test of cure.” The sample that was taken for the cytology test is also used for the HPV test.
Women with HIV
People who are HIV positive are more likely to have CIN and cervical HPV infections.
Women who have HIV are more likely to have CIN and cervical HPV infections. Because of this, all women who have just been identified should have a cervical screening, and this should be done every year after that. The age range should be the same for women who don’t have HIV. If finances allow, an initial colposcopy is also suggested.
Pregnancy
When someone is pregnant, routine screenings should be put off. If the last test was negative and then a pregnancy happens, the next test shouldn’t be put off; it should be done in the middle of the third trimester unless there is a medical reason not to.
You may also read

