First discovered in 1983 in a patient with acquired immunodeficiency syndrome (AIDs), the human immunodeficiency virus (HIV). One important component of acquired immunodeficiency syndrome (AIDs) is infection. With 35.3 million HIV positive individuals globally in 2012, the illness is a serious public health concern. HIV is treatable, albeit incurable, and clinical results are improved by early diagnosis and treatment. In 2012, there were thought to be 98,400 HIV positive individuals in the United Kingdom. Males make up the bulk of those infected in the UK (70%)
Ancestry: HIV is a member of the lentivirus family of retroviruses. Made up of an envelope, matrix, and core, it is spherical . HIV is of two types: HIV-1, the most common, and HIV-2, the less common. Further subtypes of HIV-1 exist.
Pathogenesis: The virus depletes CD4 lymphocytes, which are T helper cells. Prolonged immune system damage over time results in serious immunological deficit, malignancies, opportunistic infections (OIs), and, in the worst-case scenario, death . AIDS is the most severe stage of HIV infection and can manifest itself over a period of two to fifteen years. Not everyone who has HIV gets AIDS. A near normal life expectancy may be achieved with early diagnosis and suitable therapy.
Transmission: Blood and bodily fluids (semen, vaginal fluid, and breast milk) contain the virus.
- Sexual transmission occurs through unprotected anal, vaginal, or oral (rare) intercourse.
- Transfusion of contaminated blood and blood products; sharing injection equipment in PWIDs or in nations without sterile equipment. The UK has been screening blood for HIV since 1984.
- From mother to child vertically (antepartum, intrapartum, or postpartum).
- Exposure at work: needlestick wounds, for example.
The bulk of illnesses are contracted sexually, with MSM and those from sub-Saharan Africa being disproportionately impacted in the UK. The kind of exposure and the possibility of the source being HIV positive determine the real risk.
Primary HIV infection (PHI)
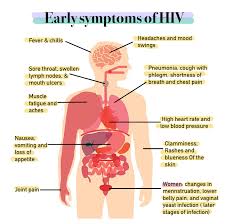
Primary HIV infection (PHI) Usually manifesting two to six weeks following infection, it is sometimes referred to as HIV seroconversion disease. More than 60% of people experience symptoms, however these are frequently non-specific and fleeting, such as pyrexia, sore throat, myalgia, exhaustion, and lymphadenopathy. Though tiredness may continue longer, symptoms last five to ten days. Mucosal ulceration of the mouth or anogenital areas and a maculopapular skin rash, especially on the trunk, are possible. It is sometimes confused with primary syphilis, other viral diseases, including glandular fever (Epstein-Barr virus).
At this point, when the virus is replicating quickly, HIV infection is most infectious.
Conditions linked to immunological weakness, such as oral candidiasis and shingles, can arise because the CD4 count can drop quickly (temporarily).
Early diagnosis reduces onward transmission by enabling prompt identification of any partners at risk. Early viral load monitoring and, when clinically appropriate, antiretroviral medication administration are also made possible by it. Should the diagnosis be overlooked at this point, it can take several years for the person to seek medical attention.
Asymptomatic HIV infection
If PHI symptoms are treated, the patient may not experience any more for several years.
The CD4 count falls yearly at a rate of about 40–80 cells/mm3 (variable).
Symptomatic HIV infection
Opportunistic infections (OIs) arise as the disease advances unchecked. OIs can be caused by bacteria, fungi, or viruses. Often, constitutional symptoms including night sweats, malaise, diarrhoea, and weight loss are linked to this stage of HIV infection. Spears, repeated episodes of seborrhoeic dermatitis, or oral hairy leukoplakia are possible.
Symptomatic (AIDs-defining) HIV infection
AIDs defining conditions include a number of infections, diseases, and cancers .
Diagnosis and investigations
Diagnosis/screening tests
- Usually, it takes 2–6 weeks to detect the p24 Ag. As antibodies form, it becomes undetectable.
- Development of HIV antibodies can take 4–6 weeks, but on occasion up to 12 weeks.
- First line serological assays, sometimes referred to as fourth generation testing, simultaneously screen for HIV antibody and p24 antigen.
- Most people who have been infected with HIV will be found by this kind of laboratory test four weeks following a particular exposure.
- Though the Expert Advisory Group on AIDS (EAGA) and BASHH advise that a negative result on a fourth-generation test conducted four weeks after exposure is highly likely to exclude HIV infection, the window period for HIV testing has traditionally been 12 weeks. Only in the case of an incident judged to have a high risk of infection is a second test at eight weeks advised.
- Patients who come in within four weeks of possible exposure should be given testing at the time of presentation and another test four weeks after the particular risk.
- Rapid point of care testing (POCT) is a method of testing a second sample after a positive HIV test; conventional testing requires processing a venous blood sample.
- POCT can provide a result in minutes using a finger prick or mouth swab sample. When venous access is limited or venepuncture is not feasible, like in outreach settings, they are helpful or when a virtually instantaneous result is desired. As POCT have a lower positive predictive value than conventional serological tests, all positive findings need to be verified on serological samples. In the UK, a legislative amendment in April 2014 allowed the sale of home testing kits “over the counter.”
Investigations for evaluating and monitoring disease - Quantitative assays of HIV RNA are viral load testing. Generally speaking, they are not utilized to diagnose HIV unless PHI is suspected and the HIV-Ab/p24Ag test comes back positive. Viral load is the measure of viral replication rate and can vary from undetectable (<50 copies/mL) to more than a million copies/mL. They are expressed on a log 10 scale, for example 106 copies/ml.
- CD4 count can rise when the viral load is reduced, like with ART.
An indicator of immunosuppression level is the CD4 count. It is typically 600–1200 per mm3 in HIV-negative people. When to start antiretroviral treatment (ART) and when to advise prophylaxis against OIs are guided by the CD4 count. - To determine how recent an infection was, avidity testing gauges how strongly antibodies attach to viral proteins. A poor avidity test is consistent with a new infection. Not many people have access to testing. It can be helpful for HIV surveillance as well as in setting a more precise time period for partner notification.
- Complete blood counts, liver and renal function tests, and HIV resistance testing should all be included of baseline testing at the time of HIV infection diagnosis. Offer STI screening that includes BBV testing.
Screening - HIV diagnosis made too late is linked to considerable and preventable morbidity and death.
- To lower the existing 25% of undetected infections, the UK Guidelines now seek to boost the use of HIV testing as well as to encourage and normalize HIV testing in situations unrelated to sexual health.
- All sexual health clinics, clinics for abortion, drug addiction programmes, and BBV services advise testing. In areas with a local HIV prevalence of more than 2 in 1000, it should also be taken into account for new patients registering in primary care and for all routine hospital admissions.
- While it’s advised, a pre-test conversation doesn’t have to be difficult or drawn out. Its goal is to provide legitimate verbal agreement for the HIV test.
- Testing should be repeated every six months for MSM and annually for PWIDs.
Testing could be a chance to implement risk-reduction strategies, such talking about safer sex, providing condoms, or getting vaccinated against hepatitis B.
Management
The complicated management of HIV patients need for a multidisciplinary approach by suitably qualified professionals. Standards of care for HIV-positive individuals have been issued by the British HIV Association (BHIVA). HIV management in detail is outside the purview of this book. Starting antiretroviral therapy (ART) depends on a number of parameters, including comorbidities, AIDS diagnosis, CD4 count (ideally before ≤ 350 cells/μL), and symptoms associated to HIV.
Antiretroviral therapy (ART)
Combining ARV drugs, antiretroviral therapy (ART) slows down HIV replication. A combination of anti-HIV medications is referred to be highly active antiretroviral therapy (HAART). Because HIV changes while it multiplies, a combination of medications is used to prevent treatment resistance. Lessening the chance of drug resistance also depends on compliance.
The area of HIV ART is developing quickly. The mode of action determines the classification of ART. There are adverse consequences connected with ART. Nausea, tiredness, skin rash, and diarrhoea are common but minor adverse effects. Drug interactions can happen and result in both higher toxicity and lower effectiveness of the drugs. Most often impacted are PIs and NNRTIs, which are metabolized through the cytochrome p450 system.
HIV and the law
Mortgages and insurance: a negative HIV test need not be revealed and should not affect anything. Positive results will have to be made public, however some businesses will provide financial goods to those who are HIV positive.
HIV transmission prosecution: HIV positive people have been successfully prosecuted in the UK on multiple occasions for giving HIV to a sexual partner (some of whom received jail sentences as a result). Scotland has a different statute than the rest of the UK in that convictions can still result even in cases when HIV is not transmitted.
Anti-discrimination laws: HIV positive people are shielded from prejudice by these laws
HIV and contraception
The health of women with HIV depends on the availability of a sufficient selection of contraceptives. Though women on ART should take particular care because of possible interactions with hormonal contraceptive methods, most contraceptive methods are appropriate for women living with HIV.
Use of condoms and another method, or dual protection, is the best method to prevent unintended pregnancy and reduce HIV transmission because, with normal use, both male and female condoms may have high failure rates for contraception. As nonoxinol-9 raises the possibility of HIV transmission, diaphragms and caps are awarded a UKMEC 3. Should permanent contraception be needed, sterilization of both sexes should be taken into consideration.
Pregnancy
- HIV can be practically completely prevented from spreading vertically. HIV mother to child transmission (MTCT) rate is about 25% when untreated.
- With interventions, this drops to less than 1%.
- Introduced in UK maternity care in 1999, universal HIV screening has proven to be a highly successful initiative with over 96% testing acceptance. The percentage of infants at risk of HIV infection has decreased as a consequence.
- Reducing the viral load (VL) to undetectable levels is the goal of ART prenatal treatment. Vaginal delivery is an option if, at 36 weeks gestation, the viral load is less than 50 copies/mL. Pre-labour caesarean section (PLCS) should be thought about in women taking zidovudine monotherapy regardless of the VL at the time of delivery and in those with a higher viral load.
- Developed nations should provide newborns with post-exposure prophylaxis. If a mother has HIV, she should not breastfeed.

