Any menstrual bleeding from the uterus that is either irregular in volume, regularity, or timing or non-menstrual is referred to as abnormal uterine bleeding (AUB). FIGO adopted the PALM-COEIN classification system for AUB in 2011.
Heavy menstrual bleeding (HMB)
Prevalence: Almost 15% of gynaecological referrals in the UK are for HMB, which affects 3% of premenopausal women.
Aetiology: Previously known as dysfunctional uterine bleeding, DUB, 40–60% of women with HMB show no uterine, endocrine, haematological, or infectious pathology on inquiry. Their symptoms are most likely the result of coagulopathy together with endometrial or ovulatory malfunction.
Determination
Pregnancy ought to be avoided in any woman of reproductive age.
History: In clinical practice, subjective assessment is utilized (clinical history); establish the type of the bleeding, i.e., frequency, duration, volume (clots, flooding, sanitary protection), cycle regularity. Objective measurement of MBL has little effect on care. Ask about related symptoms of pelvic pain or pressure consequences (gastrointestinal or genitourinary). Check the history of cervical screening.
First-line therapy can be started without the requirement for more examination or studies if the history indicates HMB without structural or histological abnormality (unless an LNG-IUS is inserted).
A history of pelvic discomfort, dyspareunia, pelvic mass, or pressure symptoms (bowel or bladder) could point to pathology, such as endometriosis, cancer, or fibroids.
Checklist
If pathology is suspected, before an LNG-IUS is inserted, or if therapy is not working, an abdominal and bimanual pelvic examination should be done. An enlarged uterine or cervical lesion has to be looked at more or, if necessary, referred.
Research on abnormal uterine bleeding
Every lady who presents with HMB should have a complete blood count.
It is only when screening is due to get a cervical smear.
Only if the personal or family history suggests it should a coagulation screen be performed.
Should the history suggest it, a STI screen (which, in the absence of examination, can be obtained by non-invasive testing)
biopsy of the endometrium
If the uterus is palpable in the abdomen, a pelvic mass is seen on vaginal examination, or medicinal therapy is ineffective, imaging should be scheduled.
First-line imaging is ultrasound. Should an ultrasound be unreliable, a hysteroscopy can be performed.
Management of abnormal uterine bleeding
Pharmaceutical treatment
Headline: LNG-IUS
Second line: COC or NSAIDs like mefenamic acid and ibuprofen
Progestogens: DMPA 12 weekly via intramuscular injection or oral norethisterone (15 mg) daily (days 5–26).
Surgical treatments
Endometrial ablations, such microwave or thermal balloon ablations. Ablation must prevent future conception.
For fibroids, uterine artery embolization or myomectomy
First-line therapy for HMB alone should not be hysterectomy.
Unscheduled bleeding on hormonal
contraception
Women should be aware of the probable bleeding patterns linked to their chosen hormonal contraceptive method before beginning use (see the contraceptive chapters). Bleeding on demand is typical during the first three to six months of hormonal contraceptive therapy. It occurs more often while using progestogen alone than when using both.
The specific mechanism of unplanned bleeding with hormonal contraceptives is yet unknown. Other disorders, such ectopy, cervical polyp, or STIs, could be at fault. Particularly if the screening regimen has been followed, cervical cancer is rare. In women of reproductive age, endometrial cancer is also rare unless there are other risk factors.
History: risk factors for pregnancy and sexually transmitted infections should be investigated and the cervical screening history verified. Find out about any other drugs you use (drug interactions are a possibility) and any related symptoms (such PCB or pelvic pain). Check that the procedure is followed (no pills missed, for example).
Examination: If cervical screening is current and there are no coexistent symptoms, examination is not necessary during the first three months of method use. Should bleeding continue for longer than three months, the lady should request an examination or cervical screening should be done. (Speculum bimanual)
Investigations: are based on the clinical results and can include an ultrasound scan, endometrial biopsy, STI screening, cervical smear, and pregnancy test.
Management: Not many possibilities. It is advisable to stick with the approach selected for the first few months rather than switching because bleeding patterns may level out. The COC may be used continuously or periodically (out with licence) for up to three months in the treatment of women utilizing progestogen-only techniques. Some people may decide to keep utilising the technique after being assured that there is no underlying disease since the benefits could exceed the drawbacks.
Postcoital bleeding (PCB)
The aetiology can be cervical polyp, cervical ectopy, invasive cervical cancer (rare), STI (such as gonorrhoea and chlamydia). About half of the women with PCB had no known cause.
Intermenstrual bleeding (IMB)
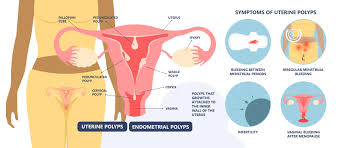
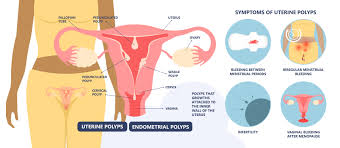
Endometrial polyps, fibroids, Cu IUD-related inflammatory response, STI-related endometritis
Assessment of PCB and IMB is the same as that of other bleeding issues (see above).
External link